Lymphoma vs Leukemia
Wondering what sets leukemia and lymphoma apart? While both are types of blood cancers, they have some pretty distinct differences that are worth knowing.
Origin of Disease
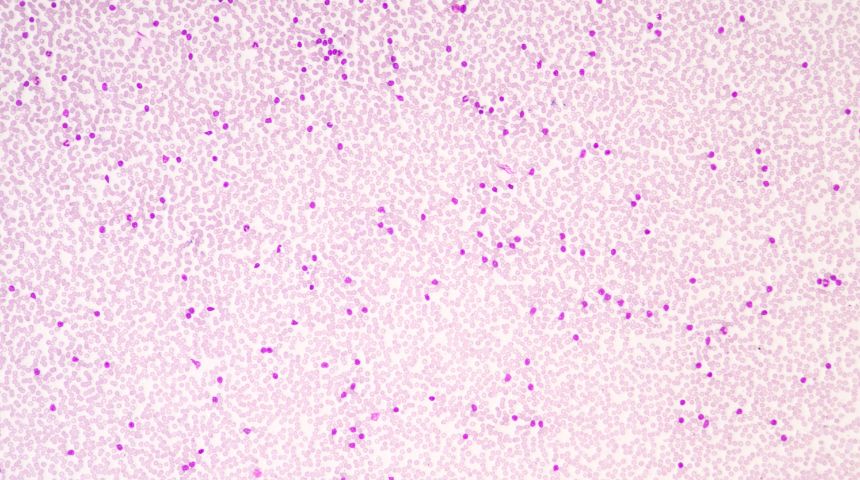
Where do these cancers start? Leukemia begins in the bone marrow. This is the soft, spongy tissue inside your bones where blood cells are made. It primarily affects the blood and bone marrow. Think of leukemia as a rogue factory in your bones that's churning out abnormal white blood cells.
Lymphoma originates in the lymphatic system, which is a crucial part of your immune system. This system includes your lymph nodes, spleen and other tissues that help your body fight infections. Lymphoma starts when lymphocytes, a type of white blood cell, start behaving badly and multiply uncontrollably.
Cell Type Affected
In leukemia, the problem lies with the white blood cells. These cells are crucial for fighting off infections, but when you have leukemia, your body starts making a ton of abnormal white blood cells that don't function properly. It’s like having an army of soldiers that can’t fight.
Lymphoma, on the other hand, specifically involves lymphocytes. These cells hang out in your lymph nodes and other parts of your lymphatic system, which is why you might notice swollen lymph nodes if you have lymphoma.
Symptoms Comparison
When it comes to symptoms, there’s some overlap, but also key differences. Both diseases can make you feel run-down and fatigued, and both can cause night sweats and weight loss. However, leukemia often leads to symptoms like frequent infections, easy bruising and bleeding because your blood isn’t working right.
Lymphoma’s symptoms are more about those swollen lymph nodes, especially in the neck, armpits or groin. You might also get fevers and have persistent itching. While both can give you fevers and make you lose weight, lymphoma’s lymph node swelling is a pretty telltale sign.
Spread and Progression
Leukemia cells can move through your bloodstream, affecting various parts of your body quickly. Because it’s in the blood, it can be a bit like a wild ride around your entire system.
Lymphoma tends to stay more localized to the lymphatic system initially but can spread to other organs if not treated. It’s more of a slow, creeping progression compared to the potentially rapid spread of leukemia.
Treatment Approaches
Chemotherapy
Chemotherapy stands as a cornerstone in the fight against leukemia and lymphoma, offering a beacon of hope for many. It utilizes a variety of drugs to target and destroy cancer cells.
You will find that the treatment is often administered in phases, starting with induction, followed by consolidation and finally maintenance. Each phase will be tailored to your unique needs. The drugs may be delivered directly into your bloodstream or, in certain cases, into the cerebrospinal fluid to reach areas that are otherwise difficult to treat.
While chemotherapy has been a game-changer, it's not without its challenges. You may experience side effects like hair loss, nausea and fatigue. You can expect your healthcare team to have these managed with supportive care.
Radiation Therapy
When it comes to treating leukemia and lymphoma, radiation therapy is a bit like a sniper ─ precise, targeted and highly effective at taking down its target. You can imagine it this way: high-energy rays, invisible to the naked eye, zooming in on cancer cells and stopping them in their tracks.
The process is like getting an X-ray but with a twist. The radiation team takes meticulous measurements to make sure they hit the right spot, using imaging tests like CT or MRI scans.
And while the treatment itself is a breeze, lasting just a few minutes, the setup is where the magic happens. They get you positioned just right, so the radiation beams can do their thing without affecting the surrounding areas.
It comes with its share of side effects, like fatigue, skin changes or hair loss in the treated area, but the trade-off is a chance to stop cancer in its tracks.
Leukemia-specific Treatment
Stem Cell Transplant
A stem cell transplant is a procedure that can be a curative measure, involving the replacement of diseased bone marrow with healthy stem cells. It essentially reboots the body's blood cell production.
It's a fascinating and complex treatment, often considered after other therapies have done their part. The process starts with a high-dose chemotherapy or radiation to clear out the existing bone marrow, making room for new, healthy cells.
Then, stem cells (those remarkable building blocks capable of becoming any blood cell the body needs) are introduced into the patient's bloodstream. These cells find their way to the bone marrow cavities, where they begin the life-sustaining task of producing red blood cells, white blood cells and platelets.
This procedure requires a stay in a specialized transplant center, where the environment is meticulously controlled to protect against infection while the immune system is down.
Lymphoma-specific Treatments
Immunotherapy
Immunotherapy is a fascinating and innovative approach to treating lymphoma. Essentially, it's like giving your immune system a training course on how to identify, target and destroy lymphoma cells.
This treatment can come in different forms, such as monoclonal antibodies that are like guided missiles, zeroing in on specific targets on the surface of cancer cells. Then there are checkpoint inhibitors, which take the brakes off the immune system, allowing it to attack the cancer more aggressively.
Targeted Therapy
Targeted therapy represents a significant advancement in the treatment of lymphoma, offering a more precise approach to attacking cancer cells. It aims to identify and attack specific cancer cell markers, sparing the normal cells.
For instance, in the case of HL, targeted therapy might be employed when the disease is advanced or if it returns after a stem cell transplant.
The beauty of targeted therapy lies in its ability to disrupt the internal signaling of cancer cells, which are responsible for their growth and division. By honing in on specific molecules within or on the surface of these cells, targeted drugs can effectively halt the progression of the disease.
The information on this website is for general educational purposes only and is not a substitute for professional medical advice. Always consult your doctor or qualified healthcare provider before making changes to your health, diet or treatment plan.